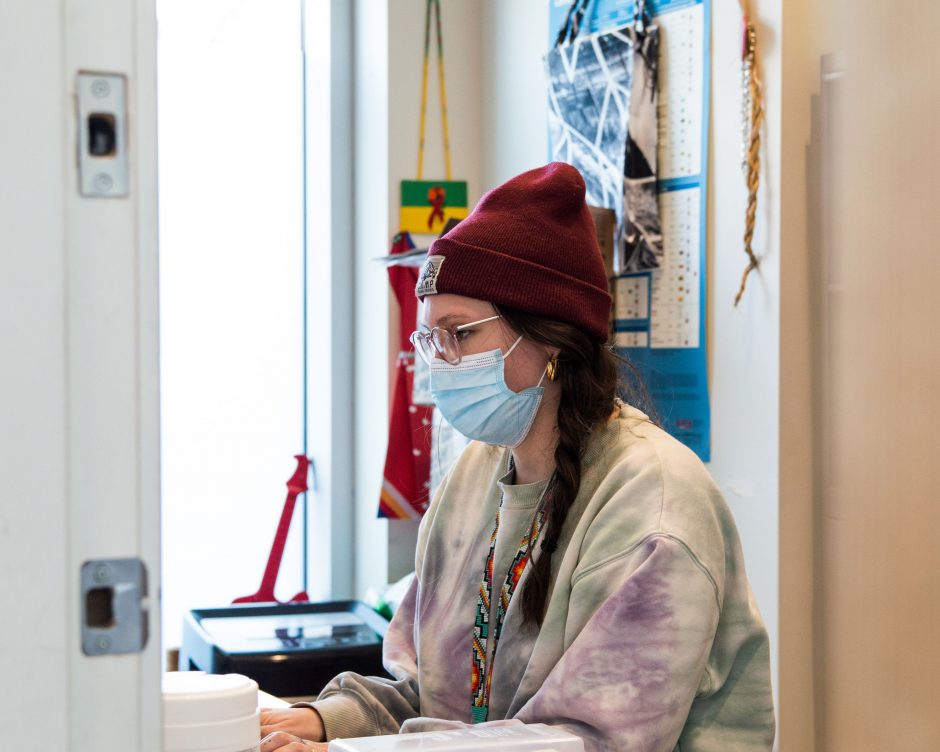
Being able to show progress is key to maintaining momentum. Staff and service users alike appreciate having input and seeing it enacted: success will breed success! Regardless of context, you should:
1. Make sure the measures and benchmarks you use are ‘equity-oriented’.
2. Use existing monitoring processes as much as possible.
3. Get a ‘baseline’ of where you’re starting on a few key indicators.
4. Include indicators of the well-being of both people using and people providing services.
5. Share data with staff.
Most health and social service settings conduct or contribute to surveys on “Patient Experiences of Care” or “Client Satisfaction.” However, these often are only completed by people with high levels of literacy, and/or with addresses and phones, for example. This can obscure the fact that some people do not have good care/service experiences. Scales that can more meaningfully tap into how all patients or clients experience your care have been developed by EQUIP Team, and there are other useful tools available.
Example:
At EQUIP we have developed a Structural Substance Use Stigma Report Card, that includes tools for collecting data from service users, service providers and at the level of the organization. Although these tools focus on promoting substance use health, they also focus more generally on promoting equity-oriented care and could be used ‘as is’ or adapted for any organization.
What data do you already collect that might be ‘equity-sensitive’? In our study of Emergency Departments, we identified the number of patients leaving without their care completed as an equity-sensitive indicator. Involving people who work with your local data in the change process can be very helpful.
Example:
In the EQUIP ED study we included staff sick time as well as staff ratings of their workplaces as provider-level indicators and the number of patients leaving without their care completed as patient-level equity-sensitive indicators . In our primary care study, we discovered that the clinics had useful data, such as social histories of foster care or residential school attendance for Indigenous people, that could signal a high potential for traumatic experiences within the healthcare system, but the data was not summarized or shared with staff. Through our research we provided trauma scores for a large sample of people accessing care, which staff found “eye-opening”, but ongoing, the clinics could use social histories as approximations of the extent of everyday discrimination and trauma experienced by people served.
Monitoring questions:
- What data do you already collect that might be ‘equity-sensitive’?
- What else could you collect to support discussions and monitor progress?
- Who is available to work with your local data to analyse and prepare useful ways to see and review it?
- How can an equity lens be useful as you review existing data or identify possible gaps in data?
- How can both service users and service provider’s experiences be tracked?