Change will look different in different contexts, depending on many factors, including the size and structure of the organization, available resources and any activities related to equity already in progress. The first four steps in the Action Kit helped you determine where things are at in your setting, and what the opportunities are to get started.
Make policy & practice changes
The discussions begun through initial educational integration sessions and ongoing opportunities for dialogue will provide many potential specific actions related to your pre-identified priorities, and likely also new ones. The Equity Committee or Working Group(s) should document and monitor these and ensure there is clarity for all involved regarding how decisions are made on what to try, and when. Communication is critical, so that people know whether and how their suggestions are taken up, and to what effect.
In addition to the ideas for action generated through the processes up to this point, other activities that can lead to concrete change include:
Examine and improve your written policies
Formal policies often operate in the background but are important in setting out what is required and possible for an organization, and how things get done. Here are some ideas of the kinds of things you can look at to ensure equity-oriented care (EOC) is always a priority:
- Mandate, Mission and Values document(s) – does what you say to the outside world align with equity goals? Is this reflected on your website or in other ways you communicate externally? This can also apply to any fundraising materials and processes, if relevant. If you are part of a larger organization, how do the statements of your organization align with what you are trying to do?
- Operational Policies – what is prioritized in these documents? what outcomes and processes are valued? Are service user voices included?
- Informal practice policies – what is valued and prioritized in these? For example, look at intake forms, referral forms and so on. What do they tell you about what is important?
- Funding Contracts – does what you commit to with funders align with equity, or present a barrier to equity goals? Can barriers be addressed?
- Your Board Policies (if applicable) – does the governance of your organization align with EOC? Are Board practices (from selection to meeting processes) equitable and representative of local communities? Is the governance model generative and open to equity?
Example:
Equity Walk Throughs can be a good time to identify ‘what’ policies should be reviewed. In one maternity care setting we worked with, the intake form was the most contentious issue identified on an Equity Walk Through. By trying to walk in the shoes of women presenting for care, staff identified that the questions they were being guided to ask women could be experienced as judgmental and even traumatizing.
Actions will arise from this review that will require additional discussion and priority-setting. These efforts will also require time, and should be staged in ways that align with your priorities, or with opportunities in the environment (e.g., are contracts being re-negotiated soon? Is the organization reconsidering their mandate? Is there Strategic Planning underway?).
Examine your protocols and procedures for service-user facing activities … AND what actually happens in practice
Some of what happens in practice will derive from the Operational Policies discussed above, but most will happen a certain way due to written and un-written policies and procedures, or because “this is the way we’ve always done things”. Several of the tools mentioned in Phase 1 can be useful here but it’s also important to take a step back and document what a typical day looks and feels like to you and those you serve, especially those who experience inequities. Some processes to examine include, but are not limited to:
- Scheduling and appointments: how does someone get scheduled for care? is there flexibility in the schedule for high needs cases, or for extra time for those who might need it?
- Arriving and waiting: the Walk Through exercise can be especially helpful here; how do people access the space? Do they have to line up (inside or outside)? Are there private spaces in which to talk? What does the space feel like for people, especially those with previous poor care experiences or who experience discrimination or stigma?
- Care encounters: are people treated with dignity (e.g., when clothing/unclothing, during physical exams), is permission sought, and are things explained before an examination or procedure? Do people get clear messages on current and next steps, taking into account various stresses on their ability to take in new information in that moment (e.g., pain, distress, trauma responses, language, cultural factors)? Are interpretation services available for people who don’t speak the language in which care is provided? If not, are there processes in place to make sure they know what to do or how to access care elsewhere?
- Exit and follow-up: is it clear whether people need to check back at reception or know how to leave and when (if necessary) to come back?
- Are the materials you share with service users available in local languages with culturally appropriate and inclusive imagery, tone and reading level? Examine your website, brochures, service user education materials, etc.
Example:
In the EQUIP primary care research, with input from reception staff on how people were received and appointments scheduled led to powerful ways to enact equity – these changes made people feel more welcome and respected and reduced their sense of feeling judged in line ups and waiting rooms.
As you can see, there are many potential directions in which your change planning and implementation activities can go. The review, planning and discussion decisions from Phase 1 will help keep you on track. We also recommend being flexible and open to adapting the plan as you identify new ideas through the education integration and policy and practice review activities in Step 4. Here are some examples of actions that can be taken:
- declarations of commitment to equity and antiracism in mission statements
- educational offerings on substance use health, harm reduction, antiracism, etc.
- group planning meetings to collaboratively decide on next steps
- informal sharing of ideas among colleagues one-to-one or in meetings
- other strategies that you know work in your context.
A cautionary note: Don’t Cherry Pick: when organizations “cherry pick” the easier aspects of the equity-oriented dimensions and related strategies, full implementation and its desired effects and outcomes are not realized. For example, sites that make their waiting rooms more welcoming with local Indigenous art (a popular strategy) but don’t foster meaningful relationships with local Indigenous communities or provide mandatory Indigenous-specific anti-racism education, are not changing anything. In fact, they may be causing additional harm by appearing to promise that things will change, when all that’s changed is the art.
Similarly, energizing direct service staff to learn how to implement trauma- and violence-informed approaches without needed changes to policy and protocols may only increase moral distress, compassion fatigue, or burnout as staff try to work in new ways without the supports required.
Below are some additional examples, organized around each EOC key dimension, of what to do and how to get started.
Examples of Trauma- and Violence-Informed Care (TVIC) Implementation Actions
Getting started on TVIC: Preparing the core implementation team
- Educate the team (Advisory Committee/Working Group(s)): take the EQUIP TVIC Foundations Curriculum to learn the basics of TVIC and become familiar with what needs to happen
- Gather relevant data on the scope and impact of trauma and violence experiences, and their effects, among those you serve
- Consider the presence and impact of vicarious trauma and moral distress among staff – how will you keep them safe through this process?
- Discuss what else is going on in the organization – are people feeling ‘change fatigue’?
- Collect any new data on TVIC and EOC to establish a baseline for your change process
Getting to work – TVIC-specific actions
- Share the data you gathered above re: trauma and violence in the lives of service users and staff
- Use the ‘Map Your Landscape Tool’ to discuss the top challenges you want to address in your Organization or Unit – from a TVIC perspective.
- Set Training Requirements and discuss which aspects are mandatory versus voluntary and within what time frame, e.g.:
- Mandatory (all current staff): TVIC Foundations, and relevant sub-modules
- Set benchmarks re: % of staff trained
- Identify, source and/or develop other resources
- Have everyone conduct, on their own, and then discuss, a Walk Through emphasizing trauma and violence informed care
- Plan dialogue sessions to embed learning in your context and surface points of resistance (link back to anticipatory guidance resources)
- Evaluate impact of training on staff, especially new understandings of trauma and structural violence and links to stigma and substance use – from judgement to compassion
- Examine existing suggestions/complaints processes; revise to include clear processes for responding to complaints; communicating clear messages about what constitutes complaints, how they are processed and handled, and what to expect when complaints are initiated
- Examine Human Resources policies using a TVIC Lens: example of revisions include:
- Assessing existing supports for vicarious trauma and moral distress (e.g., Employee Assistance Programs, supervisory practices)
- Embed interview questions that ask about understanding of trauma and violence and applications of TVIC in hiring of new staff
- Provide TVIC Training to all staff
- Implement organizational performance management processes related to TVIC, with special attention to preventing, and supporting those experiencing vicarious trauma
For more ideas about how to implement trauma- and violence-informed care, please see the EQUIP Tool: Rate Your Organization on Trauma- and Violence-Informed Care.
Examples of Anti-Racism Implementation Actions
Organizations, agencies or units that have prioritized anti-racism, including anti-Indigenous racism, recognize that it requires an ongoing process of actively working to make health and social service settings safer and more equitable for racialized and Indigenous peoples. For example, organizations, agencies or units could:
- Identify the need to address and counter racism as an explicit commitment in mission, vision, or other foundational policy statements of your organization. What are the top anti-racism challenges you wish to address in your Organization or Unit?
- Find ways to acknowledge the colonial history of Canada, e.g., feature Indigenous languages in prominent spaces/places; develop memoranda of agreement with local communities or organizations; develop anti-racism committees and anti-racism action plans, etc.
Example:
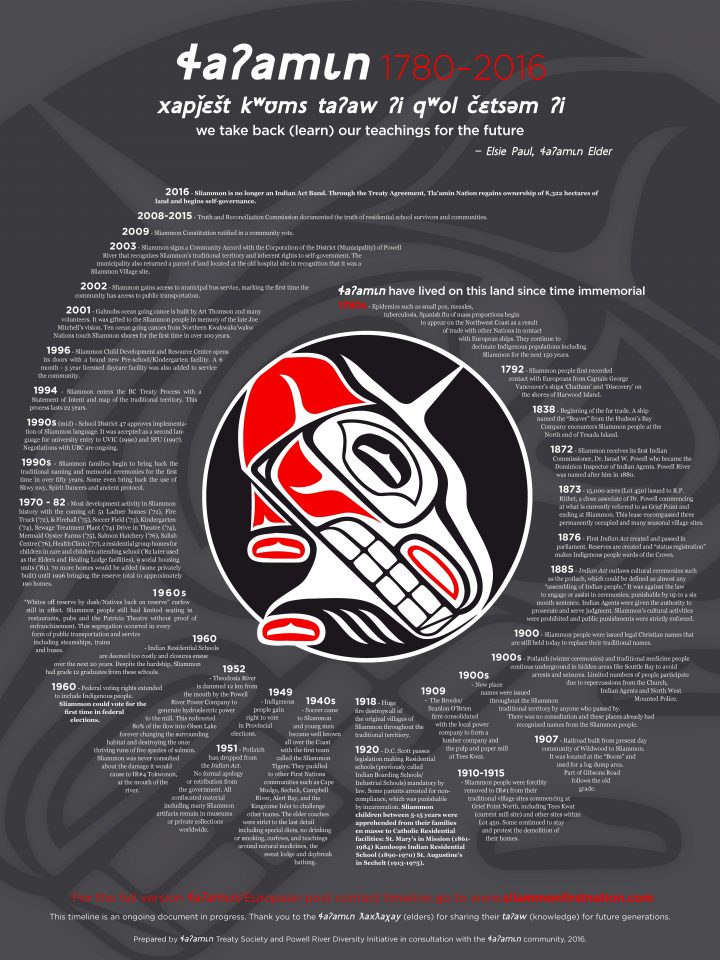
Many Indigenous communities have assembled concise summaries of colonial histories and their experiences. For example, the Tla’amin First Nation developed a visual depiction of their history, including colonial harms. A health care setting could use this “time wheel” to help non-Indigenous service providers begin to learn the history.
- Use the Map Your Landscape Tool (coming soon!) to consider: What is the role of your organizational context in creating and mitigating inequities in relation to anti-racism? What are the benefits to the organization, and to improving the health of Canadians? What are the benefits of addressing racism for the population at large?
- Implement minimum mandatory training and integration requirements on anti-racism, and voluntary training requirements and follow-up:
- Set benchmarks regarding percentage of staff trained
- Plan Integration Discussions
- Evaluate impact of training on staff
- As part of a Walk Through, conduct a security/surveillance impact assessment to raise awareness of the impact (intentionally or not) on racialized and Indigenous people coming for service; adjust security and surveillance processes in your organization/agency to mitigate negative impacts
- Examine existing suggestions and complaints processes; revise to include clear processes for responding to complaints; communicate clear messages about what constitutes complaints, how they are processed and handled, and what to expect when complaints are initiated
- Examine Human Resources policies using an anti-racism, equity, diversity and inclusion (EDI) lens: example of revisions include:
- Embedding equity-specific interview questions regarding racism into hiring of new staff – for example, asking what prospective employees know about racism or about the Truth and Reconciliation Commission report, or other relevant initiatives
- Creating an EDI recruitment plan
- Implementing performance management processes that address anti-racism and EDI considerations
Example:
Institutional-level apologies can be a start. Here’s an example from BC, where leaders of the four largest health regulatory colleges offered their apology to the Indigenous people and communities. They committed to:
- Apologize to Indigenous people for the harms suffered in a racist health-care system, acknowledging their own role
- Be anti-racist leaders who will foster a speak-up culture, where stereotypes, discrimination and racism are called out and eliminated
- Establish clear accountabilities for cultural safety and humility within our leadership teams.
These apologies must be backed up by clear and concrete collaboratively designed, appropriately-resourced and implemented action plans.
For more ideas about how to address Anti-Indigenous Racism, please see the EQUIP Discussion Tool: Rate Your Organization on Addressing Anti-Indigenous Racism.
Examples of Harm Reduction and Substance Use Health Actions
Getting started on substance use stigma toward substance use health and harm reduction
As with any of the key dimensions, how to get started varies with where you are starting. With respect to harm reduction, has your setting:
- Fully committed and resourced itself for harm reduction?
- Committed to harm reduction on paper, without necessarily having meaningful resources and strategies in place?
- Not yet explicitly examined its stance?
Example:
In one of the primary care organizations we worked with, the organizational mission and mandate expressed commitment to harm reduction. However, staff did not know exactly what harm reduction was, and could not identify ‘how’ the commitment was being enacted. The organization then worked over a number of years to develop policies and practices and provide staff education to support operationalizing harm reduction.
First, take stock of your organization’s stance toward substance use, and then the stance of diverse individuals within the organization. Take stock of the resources you have toward harm reduction (e.g. experts, people with lived experience, policies that are already in place).
Next, build on those resources. Most communities have a range of experts that may include street nurses, overdose prevention personnel, groups of people with lived experience, among others. Engage their expertise to further assess your approach and identify priorities.
In a recent partnership with a small rural-serving hospital in Port Alberni, BC, we had the opportunity to observe as staff worked through “Step Zero”, and to engage with community partners who had expertise to help guide their work toward a “substance use health” orientation to care.
Most health and social service settings will find partnerships invaluable to guide change and connect to resources. Some actions might include:
- Creating partnerships with community organizations serving people who use substances
- Creating safe spaces for people to use substances while they are receiving care
- Educating staff on substance use stigma: substance use does not mean violence; judgement and poor treatment contribute to violence
- Instituting a “substance use health” orientation throughout the organization
- Instituting policies so that people are not discharged for using substances, and are not discharged with prescriptions for lower doses of opioid replacement than they are used to
- Training staff on the use of destigmatizing, person-first language
- Reviewing how security and surveillance are deployed in relation to people perceived to be using substances in “socially unacceptable” ways
- Reviewing documents with a strengths based anti-stigma lens; EQUIP has created an Equity-Oriented Opiate Treatment Agreement, which your team can draw on
- Replacing stigmatizing and harmful policies and signage with messages of welcome and non-judgement
- Consider how to integrate attention to substance use health into care plans and processes
- Provide easily accessible harm reduction supplies: food, water, safe use supplies, sharps containers, etc.
- Provide signage and information to support access to external resources.
For more ideas about how to address Harm Reduction / Substance Use Health, please see the EQUIP Tool: Rate Your Organization – Harm Reduction and Reducing Substance Use Stigma.
A note on what to do when people resist change:
As mentioned in the Introduction to this Action Kit, change is not easy, and you can anticipate various forms of overt and less obvious resistance or changes, or to the kinds of discussions that are inevitable when considering how to implement EOC. To be effective, actions must necessarily be disruptive and challenge existing structures that work quite well for some people but poorly for others. People will feel challenged and even distressed by changes, including both those who do not see everyone as ‘deserving’ and those who feel uncomfortable about their own previous practices. This is all part of change – if nothing changes, nothing changes!
Example:
Sometimes more severe actions are required. For example, in one of the primary care settings with which we worked it became very evident that one of the service providers was actively racist toward patients. The management and Board had to take action to have the person removed from employment.
We have created a tool called Ensuring Momentum & Accountability: Countering Resistance to Equity Actions that outlines what resistance can look like and how to anticipate and counter it in ways that will bring people along at their own pace, while not delaying or derailing your equity initiatives.